
The ITC provides all young transplant physicians and nurses working in the field of transplantation with a broad and concise overview of all relevant topics in HSCT. The lectures were comprehensive and informative, presented by experts in their respective fields.
A group of past Young Ambassadors and nurses agreed to chronicle some keys sessions from both the physicians and nurses’ programme. You can read their full reports below.
Physician Programme – Wednesday, 4 November 2020
Session I
Summary by Yuliya Rogacheva, R.M. Gorbacheva Memorial Institute of Children Hematology and Transplantation, St. Petersburg, Russia
The first session was focused on the problems of donor selection, techniques and options for mobilizing peripheral blood stem cells as well as methods of cell processing and preservation and cell engineering.
Prof. Loiseau reported on the principles of donor selection for allogeneic hematopoietic stem cell transplantation (allo-HSCT). The procedure of transplantation from an HLA-incompatible donor with focus on haploidentical HSCT, which is especially relevant during the COVID-19 pandemic, was also highlighted. Prof. Loiseau threw light on the importance of detecting donor-specific antibodies during haplo-HSCT such as intra familial HLA immunization that occurs frequently (10-20%). Highly relevant topics such as donor-specific antibodies (DSA) and desensitization methods were actively discussed during the report.
Prof. Duarte highlighted the methods of mobilizing blood stem cells for apheresis, compared the modes of chemo-based mobilization, as well as steady state. Interesting data on how we should manage poor mobilisers, especially role of plerixafor, were presented.
Prof. Chabannon covered how bone marrow cells are directly harvested, talked about peripheral blood stem cells topic, and shed light on the collection of immune cells. Report included not only apheresis but also measuring the content in immune effector cells. It was also important that Prof. Chabannon highlighted the need to distinguish between the principles of cell engineering and major products. He also covered the topic of minimally manipulated cells products like red blood cell depletion, plasma removal and immune cell depletion, which is sometimes necessary to perform a successful HSCT.
Session II
Summary by Yasmina Serroukh, Bone marrow and cellular therapy department. Hôpital Maisonneuve-Rosemont, Université de Montréal, Canada
First, Prof. Chabannon highlighted that the selection of qualified CAR-T cell centers is a complex process involving pharmaceutical companies, health authorities, accreditation bodies and academia. The common goals of these actors are to optimize the logistic, scientific and clinical aspects of CAR-T cell therapy.
Then, Prof. Urbano-Ispizua summarized that chimeric antigen receptors (CAR) include an antigen-binding domain, coupled with an intracellular CD3-signal and a co-stimulatory molecule. Autologous T cells are activated in vitro, transduced with the CAR genetic construct using viral vectors and expanded to generate a sufficient amount of tumor-specific cytotoxic effectors. CAR-T cells targeting CD19 are approved for lymphoid malignancies and growing evidence should lead to approval of BCMA-directed CAR-T cells for multiple myeloma in the coming months.
Next, Prof. Kuball stressed on lymphocytes mediating graft versus tumor effect and immune reconstitution but also graft versus host disease. T cell composition can be modulated ex vivo by selective depletion or in vivo by optimizing lymphodepleting conditioning and/or use of post-transplant cyclophosphamide. Post-transplant donor lymphocyte infusions (DLI) can be used pre-emptively based on measurable residual disease or chimerism while therapeutic DLI are used for relapse in combination with chemotherapy.
Finally, Prof. Mohty showed that the conditioning regimen is a combination of chemotherapy and/or radiation with anti-tumor activity and immunosuppressive properties to prevent rejection. Conditioning intensity depends on the degree of myeloablation provided. Full myeloablative regimens offer faster anti-tumor effect but higher toxicity while non-myeloablative regimens rely on a delayed graft versus tumor effect with better tolerability. A broad spectrum of conditioning intensity allows adaptation to patient- and disease-specific factors to achieve the best transplant outcomes.
Session III
Summary by Yasmina Serroukh, Bone marrow and cellular therapy department. Hôpital Maisonneuve-Rosemont, Université de Montréal, Canada
First, Prof. Zeiser gave a compelling overview of the pathophysiology of acute graft-versus-host disease (GVHD). This disease is triggered by conditioning-induced tissue damage. Activated antigen presenting cells (APCs) interact with donor T cells. Upon activation these T cells produce pro-inflammatory cytokines responsible for the clinical picture. Mesenteric neutrophils and microglia can also mediate GVHD through local antigen presentation.
Next, Prof. Malard showed that standard acute GVHD prophylaxis combines a calcineurin inhibitor (CNI) and methotrexate. Mycophenolate-mofetil (MMF) can be combined with a CNI for reduced-intensity conditioning transplant. Anti-thymocyte globulin added to the conditioning regimen lowers incidence of GVHD. Post-transplant cyclophosphamide is the standard GVHD prophylaxis for haploidentical transplants. Treatment of acute GVHD is methylprednisolone at the dosis of 1 mg/kg for grade I-II or 2 mg/kg for higher grades. Ruxolitinib is the only approved second line treatment. Many other options are available or in investigation.
Third, Prof. Penack summarized the decision process regarding chronic GVHD. Decision to treat chronic GVHD should be based on a balance between risks and benefits and follow published definitions and response criteria. Standard first line is 1mg/kg oral prednisone for at least one month. The combination of fluticasone, azithromycin and montelukast is recommended in case of demonstrated lung involvement. Physicians should follow local guidelines and include patients in studies when available.
Last, Prof. Greinix gave an important overview of the role of supportive care in refractory settings of patients with GVHD. Supportive care is a key component of GVHD management. It includes the prevention of complications, symptoms control and minimization of systemic immunosuppression. It should be global, patient-centered and multidisciplinary with the objective of improving patients’ quality of life.
Session IV
Summary by Abdul Hamid Bazarbachi, 1st year resident in the "Department of Internal Medicine, Jacobi Medical Center, Albert Einstein College of Medicine, New York, USA
Allogeneic stem cell transplantation (allo-SCT) is a complex therapy with a sequelae of complications secondary to drug toxicities, immune suppression, and graft-vs-host disease (GVHD). Dr Carreras focused on early and rare complications post allo-SCT, focusing mainly on the vascular endothelial syndromes including veno-occlusive disease/sinusoidal obstruction syndrome (VOD/SOS), capillary leak syndrome, thrombotic microangiopathy (TMA), diffuse alveolar haemorrhage, and engraftment syndrome. These complications are all thought to originate from endothelial damage at the capillary level in the setting of the triad of endothelial activation, procoagulant state and increased permeability, and their diagnosis and treatment can be challenging given their overlapping clinical presentations. Dr Carreras explained the pathophysiology behind these entities including the three-hit hypothesis and role of IL-8 in neutrophil activation and release of neutrophil extracellular traps in the development of TMA. He highlighted the defining features and diagnostic criteria of each of these entities such as the recently updated EBMT criteria for the diagnosis of VOD/SOS. He also went over the different treatment approaches currently available and stressed the importance of high vigilance for these conditions as one of their most common features is eventual multi-organ failure due to treatment delay. Dr Peric’s talk shifted focus to late complications of allo-SCT, emphasizing that despite surviving beyond 2 years of allo-SCT, overall survival remains considerably lower than that of the general population. The biggest culprits for increased mortality are relapse, cardiovascular disease, secondary neoplasms, loss of bone density, endocrinopathies, chronic GVHD and chronic immunosuppression. Dr Polomeni further alluded to these complications with her talk focusing on long-term quality of life (QOL) and psychosocial aspects of allo-SCT such as complaints of fatigue, sexual dysfunction, anxiety and depression that patients experience decades post allo-SCT. Mr Bouguet, a lymphoma survivor, concluded the first part of the session with a very moving talk about his personal experience fighting follicular lymphoma, how he needed someone to trust to “pilot his plane to safety” through his journey, and provided insight into the multidimensional impact his disease had on every aspect of his life.
The second part of the session focused on infectious complications post allo-SCT, starting with fungal infections by Dr Styczynski. His lecture focused on the principles of diagnosis, prophylaxis and treatment of invasive fungal diseases (IFD), including management of Aspergillus, Candida and Mucor all of which account for over 90% of IFD cases. He presented the recently updated definition of IFD to distinguish between proven, probable and possible IFD, and highlighted the importance, indications and limitations of diagnostic biomarkers, molecular techniques and imaging for early and accurate diagnosis. His talk then shifted to the indications and patient-specific approach for prophylactic antifungal use in different settings, as well as treatment indication with respective recommendation grades. Dr Ljungman then followed with his talk on viral infections. He emphasized pre-transplant risk assessment and the importance of post-transplant monitoring and preemptive treatment. Regarding the classic offender, CMV, there remains significant controversy around the use of prophylactic versus preemptive treatment in management. Dr Ljungman also discussed HSV/VZV, both of which warrant long-term prophylaxis as well as preemptive use of rituximab for patients at high risk of EBV reactivation. He concluded his talk with respiratory viruses such as adenovirus and influenza, and the challenges that COVID-19 has resulted in for allo-SCT. Finally, Dr Averbuch went over the most prominent bacterial infections post allo-SCT, highlighting the wide range of reported infection rates across centers depending on different infection control strategies and risk factors for developing severe bacterial infections. Dr Averbuch stressed the imminent dangers of antibiotic resistance given the alarming rates of increased multidrug resistance. She explained that appropriate therapy initiation is crucial whereby delay of appropriate antibiotics results in worse outcome and discussed the treatment approach to febrile neutropenia including indications for an escalation versus de-escalation strategy. Finally, she went over some of the newer agents available and presented data of their respective efficacy and optimal treatment duration.
Physician Programme – Thursday, 5 November 2020
Session V
Summary by Razan Mohty, 3rd year hematology/oncology fellow, chief fellow, at the American University of Beirut Medical Center, Beirut, Lebanon
Despite the advances in the treatment of hematologic malignancy, allogeneic stem cell transplantation (allo-SCT) remains a major player in the therapeutic algorithm of these patients, particularly those with high-risk disease. In this section, Dr Sierra discussed the role of allo-SCT in acute myeloid leukemia (AML). In 2020, allo-SCT is strongly indicated for young and older fit AML patients with intermediate and high-risk disease who achieve complete remission (CR) after induction therapy. Dr Sierra reviewed studies on the best conditioning regimens, donor selection, and optimal GVHD prophylaxis, with emphasis on maintenance therapy as a strategy to prevent relapse. In the second part of this section, Dr Craddock summarized strategies to improve AML patient outcomes after transplant notably by achieving minimal residual disease (MRD) negativity prior to allo-SCT, improving conditioning regimens, tailoring GVHD prophylaxis, and most importantly by incorporating a post-transplant maintenance strategy using hypomethylating agents and FLT3 inhibitors in FLT3 mutated AML. The third speaker, Dr Yakoub-Agha summarized allo-SCT recommendations in myelodysplastic syndrome (MDS). He mentioned that allo-SCT is strongly indicated for high- and very-high risk MDS according to the revised IPSS-R score and in intermediate-risk disease with higher risk features. Also, in MDS, haploidentical stem cell transplantation is increasingly used. In parallel, bridging therapy to upfront allo-SCT with hypomethylating agents is indicated if allo-SCT is delayed for more than 4 months after diagnosis. He added that despite advances in the conditioning regimens and strategies to decrease disease burden prior to allo-SCT, the outcome of patients with poor cytogenetics is still dismal. In the last part of this section, Dr Nagler summarized allo-SCT indications for acute lymphocytic leukemia (ALL) patients. In brief, allo-SCT is still indicated in CR1 in Philadelphia (Ph)-negative ALL who remained MRD positive or who have pre-treatment high-risk features, and in Ph-positive ALL. In the relapsed/refractory setting results are poor. In patients with low-risk Ph-negative ALL, allo-SCT is deferred to the CR2 setting. Dr Nagler tackled the different conditioning regimens used and transplant outcomes, stressing on the importance of MRD negativity prior to transplant as a major factor affecting outcomes. Also, he added studies on the use of CAR T-cells as a bridge to allo-SCT. He concluded that with the advances in the treatment of ALL, particularly with the development of new monoclonal antibodies, transplant indications for ALL might change.
Session VI
Summary by Claire Horgan, Paediatric haematology registrar, Birmingham, UK
Régis Peffault de Latour started the session discussing transplant indications for bone marrow failure. He highlighted the importance of early SCT in those with SAA, ideally within 3 months of diagnosis with a matched sibling donor. The use of MUD upfront is increasing and there are ongoing trials looking at haplo and cord transplants. Bone marrow grafts should be used along with RIC regimens to minimise toxicity. IST remains standard 1st line treatment in the over 40s, however, MUD SCT is a superior option to a 2nd course of IST in suitable individuals following IST failure. When transplanting in Fanconi Anaemia and DKC, it is essential to ensure that family donors are systematically screened and long-term follow up is crucial due to the risk of secondary malignancies.
Next, Arjan Lankester discussed the current state and challenges for HCT in inborn errors of immunity, in which significant advancements have occurred over the past few decades. The aim of HCT in these patients is to replace dysfunctional haematopoeitic cells and cure, alleviate, or prevent cell-related disease manifestations. Improvements in the transplant process over recent years, along with developments in genetic tools to aid early diagnosis, have resulted in SCID transplant survival rates now approaching 90% with matched donors.
Selim Corbacioglu concluded the session discussing transplant for haemoglobinopathies. MSD is the standard of care in both B-thalassaemia and sickle cell disease and should be done as early as possible. Haplo HCT is curative and comparable to MSD, with PT-Cy being a cost efficient and affordable option in low- and middle-income countries, hence the classical donor hierarchy can be challenged depending on cost, availability and logistics. Gene therapy is likely to become a significant part of clinical practice in the years to come.
Session VII
Summary by Nico Gagelmann, University Medical Center Hamburg-Eppendorf, Department of Stem Cell Transplantation, Hamburg, Germany
Prof. Kröger showed that 60% of myelofibrosis patients may be cured after allo-SCT. Intermediate-2 and high risk according to DIPSS clearly benefit from allo-SCT. Younger patients with intermediate-1 risk should be considered if they have refractory anemia or adverse genetics. Transplant-specific risk using the MTSS should be part of the decision making. For secondary leukemia, patients with complete remission may be rescued.
Prof. Montoto reported that auto-SCT is still the first line option in mantle-cell lymphoma with complete/partial remission after cytarabine/rituximab induction. A current trial evaluates first line treatment comparing auto-SCT versus auto-SCT/ibrutinib versus ibrutinib. At relapse, auto-SCT is indicated in diffuse large B-cell lymphoma/follicular lymphoma. Allo-SCT may be indicated only after an auto-SCT in NHL.
Prof. Glass showed that current CD19-directed CART therapy achieves remissions in 50-80% of refractory NHL, with long-term survival in 30%. High active lymphoma mass is a significant predictor for worse outcome. Acute toxicity and prolonged neutropenia will need special treatment algorithms but can be controlled for. CARTs are second line treatments, enhanced by new drugs as bridging therapies.
Prof. Sureda underscored that auto-SCT is considered the standard of care for HL presenting with primary refractory disease or relapse after first line therapy. Allo-SCT it is a valid treatment option for patients failing auto-SCT, while the inclusion of new drugs such as checkpoint inhibitors consistently replace treatment sequences and can be safely combined with an allo-SCT.
Last, Prof. Bladé underlined that auto-SCT is the standard of care for younger patients with multiple myeloma. In the elderly, selection is crucial. Tandem auto-SCT seems beneficial in patients with high-risk cytogenetics. Second auto-SCT may be considered in patients with long-term remission after first auto-SCT. The indications for allo-SCT may be: early relapse (<24 months after auto-SCT, unfavorable cytogenetics, extramedullary disease).
Session VIII
Summary by Claire Horgan, Paediatric haematology registrar, Birmingham, UK
Christina Peters started the session with an overview of the state of the art of transplantation in childhood leukaemia and presented the results of the ALL SCTped FORUM study. This demonstrated significantly improved OS and EFS at 2 years with TBI/etoposide Vs myeloablative chemo conditioning as a result of higher relapse incidence in the patients who did not receive TBI. Subgroup analysis failed to establish a subset of patients in which TBI could be omitted.
Allogeneic transplant in AML is used to sustain remission for high risk patients. The optimal conditioning regimen continues to be a matter of debate, however myeloablative conditioning is superior to RIC in children and conditioning should not include TBI. Prospective multicentre studies are needed.
Next, Rafaella Greco discussed transplant in autoimmune diseases which are the fastest growing indication for transplantation in the EBMT registry. Autologous HSCT enables ‘debulking of inflammation’ with cytotoxic therapy followed by ‘resetting/rebooting’ the immune system, whilst allogeneic HSCT offers immune replacement and a ‘graft versus autoimmunity effect’ in these patients. Careful selection of patients taking into account the disease, risks vs benefits, and expertise of transplant centre is essential.
Harry Dolstra then discussed combining cellular therapy and HSCT including the potential role for allogeneic NK cell therapy against AML and MDS. Several developments are ongoing with cellular therapies that can be applied pre- and post-transplant, however, complexity and precision needs to be managed along with costing, sustainability and availability.
Prof. Orchard concluded the session with a talk on JACIE and quality markers in HSCT, highlighting how important the role of quality assessment and management is in all stages of the stem cell transplant process. JACIE standards provide an operational structure for HSCT teams and quality is essential to the creation, implementation and maintenance of these standards.
Nurses Programme - Friday, 6 November 2020
Sessions I and IV
Summary by Sandra Schönfeld, Member of the Nurses Group Scientific Committee; Clinical Nurse Specialist Haematology- Basel, Switzerland
The ITC Nurses Programme started with an amazing session that addressed different essential topics in transplant nursing: psychosocial care, palliative care, disaster management and considerations for the minor.
Angela Scherwath, working as a psychologist in haematology at the University Hospital in Hamburg in Germany, identified in her speech important barriers for nurses to psychosocial care and addressed them with practical tips that can easily integrated in daily care. An important tip in this view is that we do not have to be afraid of not being the right person to provide good psychosocial care. We should be confident that we are the right person. This was followed by an impressive talk from Ruth Ting, a palliative consultant at the King‘s College Hospital in London, highlighting that palliative care is an holistic approach that is not only a specialty in medicine. On the contrary, it can be applied by every healthcare provider. Her tips for dealing with palliative patients were backed up with practical examples and showed impressively what simple methods make dealing with palliative patients easier. My personal Take home message is a quote from her that made me very thoughtful: “Death is not a medical failure, it is biological certainty. Poorly managed death is a medical failure.”
The last session of the Nurses Programme set highlights on different complications in haematology, including the rare complication of VOD (veno-occlusive disease) which is often difficult to handle for nurses. A case report showed the complexity of VOD and the multidisciplinary approach which is essential in caring these patients. This presentation was followed by a speech from Iris Agreiter, working at the St. James‘s Hospital in Dublin, focusing on viral illnesses, how to monitor them and different treatment options. She highlighted the patients‘ perspective which is often neglected in nursing. The very last talk of this day was from Michelle Kenyon, working at the Department of Haematological Medicine at the King‘s College Hospital in London, was about late complications and Quality of Life issues after transplantation. She highlighted that patients after stem cell transplantation suffer from a broad range of difficulties that have to be addressed. This can be challenging as the needs of these patients should be embedded in a long-term setting. However, long-term care is often integrated into an acute care setting that cannot always meet these needs. My personal highlight in this session is the reflection on this long-term care and that these patients need an appropriate follow-up that includes a relationship between the patient and the healthcare provider which is based on trust that patients can express their needs.
Sessions II and III
Summary by Janet Baker, Member of the Nurses Group Scientific Committee; Apheresis Clinical Nurse Specialist- Bud Flanagan Apheresis Unit- Haemato-Oncology - The Royal Marsden NHS Foundation Trust
The 2020 EBMT International Transplant Course Nurses Programme was very successfully and provided a broad range of relevant topics and speakers reflecting the pivotal issues in Stem Cell transplant nursing.
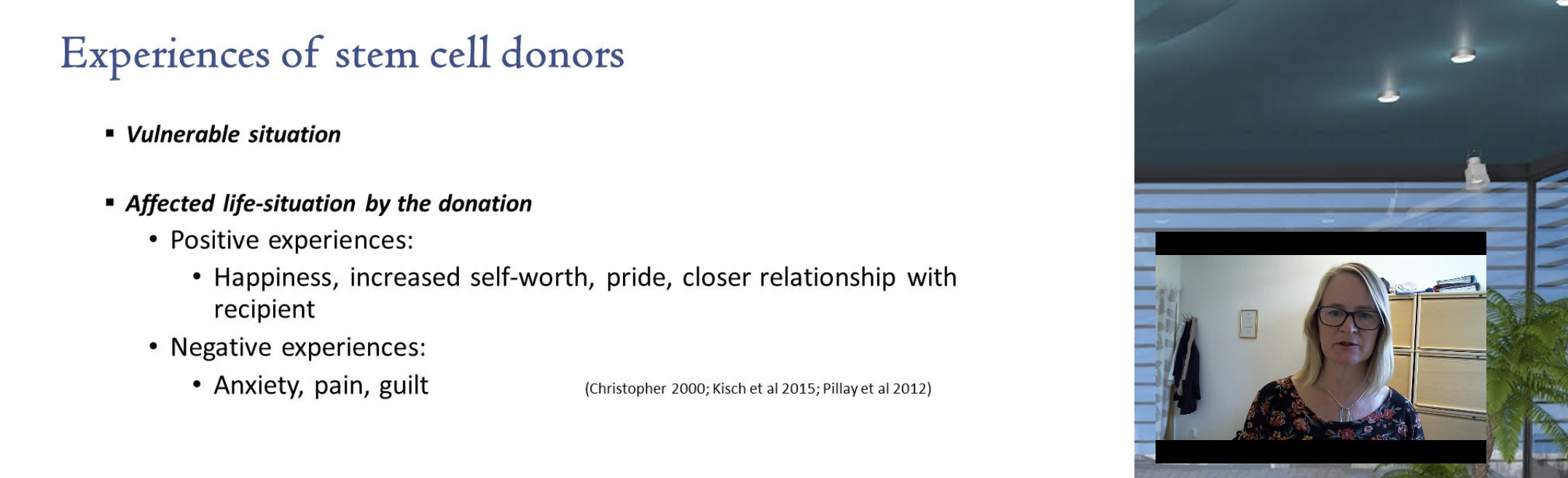
One of the highlights was the session ‘Donors, how will we care for them?’. Annika Kirsch from Lund in Sweden presented a thought provoking and informative overview of the experience and outcomes of related donors, a group which is often not well explored. Annika expertly highlighted the fundamental concepts of free choice, the right to refuse, and that allogeneic donor suitability should always be evaluated by an HCP who is not the primary HCP overseeing the care of the recipient. These are now underpinned by JACIE standards. She introduced to us the Information and Care Model implemented in her centre which is a structured framework to care for related donors, involving education, support, and follow up. She concluded with some powerful quotes from donors from her own research which emphasised some of the ethical, moral, and psychological dilemmas inherent in the donor experience. Annika’s take-home message was: ‘Don’t forget the donor in the HSCT process’.
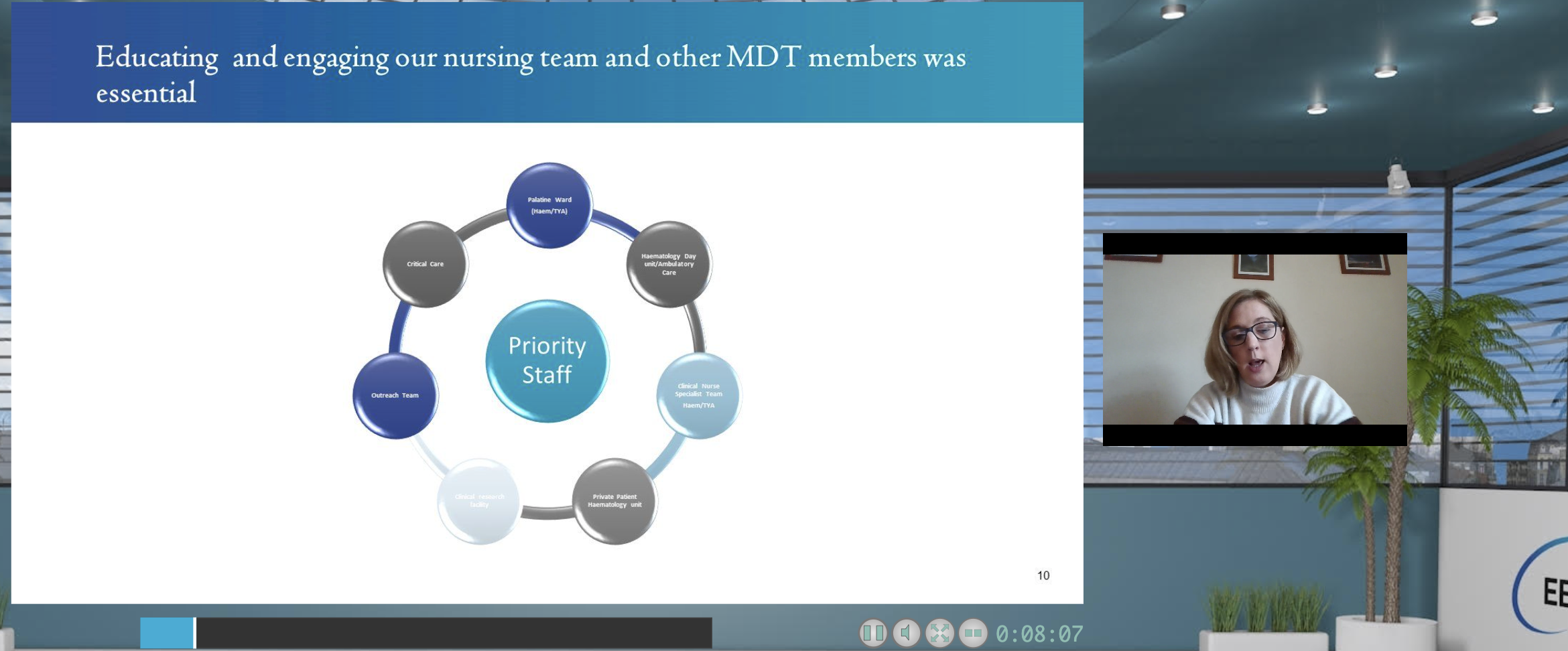
Another very topical and pragmatic session was Ruth Clout’s ‘CAR-T training: a nurse’s perspective’. Ruth is a Practice facilitator at the Christie hospital in the UK and a large part of her role within the last few years has been preparing, training, and educating nurses, and other HCPs, to be able to care for patients receiving CAR -T therapy. She provided a thorough overview of how this was achieved, and is still being delivered despite study/meeting restrictions imposed by Covid 19. This involved varied methods of delivery including on-the job training, joint multi-disciplinary learning, additional study days incorporating JACIE standards, and additionally an academic component in collaboration with Manchester University. Ruth highlighted how apprehensive nurses were in anticipation of this new treatment but following education and training, feedback and observation suggests these nurses now care with confidence for this new patient cohort. Ruth’s take home message was: ‘Learn from and collaborate with other centres and nurses’.
My take home message: a participant contacted myself and another audience member after the nurses meeting day following a discussion in the Q & A session, proof that net -working and sharing of practice is still possible in the virtual conference format!